Pancreatic inflammation characterizes acute pancreatitis, a sudden and possibly fatal illness. This important organ is essential for digestion and blood sugar control. Numerous serious signs and problems might develop as a result of pancreatic inflammation. We will examine the causes, signs, symptoms, diagnosis, and available treatments for acute pancreatitis in this extensive post.
I. Pancreas Anatomy and Function
Let’s take a moment to comprehend the architecture and functions of the pancreas before delving into acute pancreatitis.
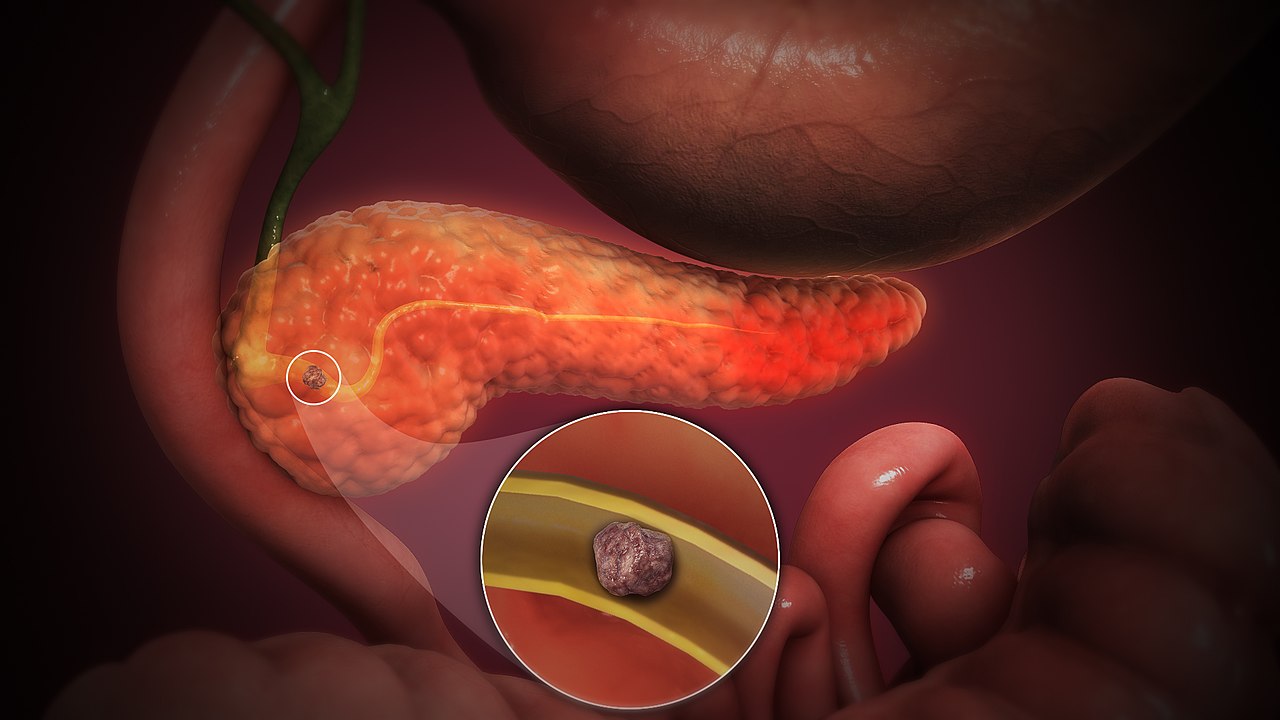
Behind the stomach, tucked between the spleen and the duodenum (the first section of the small intestine), is the glandular organ known as the pancreas. It accomplishes two major goals:
Exocrine Function: To aid in the breakdown of food, the pancreas secretes digestive enzymes into the small intestine. These enzymes facilitate the breakdown of proteins, lipids, and carbohydrates.
The pancreas also has clumps of cells known as the Islets of Langerhans, which produce hormones including glucagon and insulin. These hormones control blood sugar levels, enabling the body to utilize glucose as an energy source.
ExoII. Acute Pancreatitis: What Is It?
An rapid pancreatic inflammation known as acute pancreatitis can range in severity from moderate to severe. This disorder develops when pancreatic digesting enzymes that are ordinarily dormant become prematurely awakened, harming pancreatic tissue.
3. Acute Pancreatitis Causes
Acute pancreatitis can be brought on by various factors, such as:
Gallstones: Gallstones are one of the most frequent causes of acute pancreatitis. They can clog the pancreatic duct and cause inflammation.
Chronic and excessive alcohol use can irritate the pancreas, which increases the risk of acute pancreatitis.
Trauma: The pancreas can become damaged and inflamed as a result of physical harm to the abdomen, such as from a fall or a car accident.
illnesses: In rare instances, both bacterial and viral illnesses, such as the mumps, can cause acute pancreatitis.
Drugs: Some drugs, particularly those that have an impact on blood lipid levels or are used in chemotherapy, might cause pancreatitis.
Hypercalcemia (high blood calcium levels) and hypertriglyceridemia (high blood triglyceride levels): These disorders can raise the risk of acute pancreatitis.
Genetic Factors: In some situations, hereditary diseases or genetic mutations can increase a person’s risk of developing pancreatitis.
IV. Acute Pancreatitis Symptoms
There are a number of symptoms associated with acute pancreatitis, and their severity might vary. Typical signs include:
Acute pancreatitis is characterized by severe abdominal pain that is persistent and intense, frequently originating in the upper abdomen and radiating to the back. After eating, the pain could get worse.
Vomiting and Nausea: People with acute pancreatitis frequently feel queasy and may vomit.
Low-grade fever: This symptom is frequently present in addition.
Rapid Pulse: Tachycardia, or an elevated heart rate, may be seen.
Jaundice: If the bile duct is inflamed, yellowing of the skin and eyes (jaundice) may result.
Acute pancreatitis can cause hypotension (low blood pressure) in severe cases.
Breathing Issues: If the inflammation spreads to the lungs, breathing issues may develop.
Shock: Severe cases of acute pancreatitis can result in shock, a potentially fatal disease in which important organs lack sufficient blood flow and oxygen.
If you or someone you know has severe abdominal pain or any of these symptoms, you must see a doctor right once because acute pancreatitis can develop quickly and cause life-threatening consequences.
Diagnose Acute Pancreatitis, Chapter V
Typically, a medical history, physical examination, and diagnostic testing are used to diagnose acute pancreatitis. The following techniques are frequently employed:
Medical History and Physical Exam: The healthcare professional will ask the patient about their symptoms and conduct a physical exam, paying particular attention to abdominal discomfort and jaundice symptoms.
Blood testing: Blood testing are critical in the pancreatitis diagnosis process. Increased levels of pancreatic enzymes like amylase and lipase are a sign that the organ is inflamed.
Imaging Studies: A number of imaging examinations, such as:
An abdominal ultrasound is a non-invasive examination that can detect gallstones or enlargement of the pancreas.
Computed Tomography (CT) Scan: CT scans offer fine-grained images of the pancreas and other structures that can be used to assess the condition’s severity.
Using magnetic resonance imaging (MRI), the pancreas and ducts can be seen.
Endoscopic Retrograde Cholangiopancreatography (ERCP): An ERCP may be carried out in certain circumstances to assess the pancreatic and bile ducts. Additionally, it can be utilized for medical treatments, such as eliminating obstruction-causing gallstones.
VI. Acute Pancreatitis Complications
Numerous complications, some of which may be fatal, can result from acute pancreatitis. These difficulties comprise:
Pancreatic Necrosis: In severe circumstances, the inflammation may result in the pancreas’ tissue dying (necrosis).
Pseudocysts: The pancreas may develop pseudocysts as a result of fluid and material buildup.
Pseudocysts and regions of pancreatic necrosis can get an infection, which is a significant side effect.obstruction.
Internal bleeding can occur when blood vessels in the pancreas break.
Respiratory Distress: Respiratory distress syndrome can develop as a result of severe acute pancreatitis’ impact on lung function.
Acute renal injury can result from acute pancreatitis, which can also compromise kidney function.
Diabetes may result from pancreatic damage that affects the organ’s capacity to make insulin.
VII. Acute Pancreatitis Treatment
The severity and underlying cause of acute pancreatitis determine how it should be treated. The main elements of treatment are as follows:
Hospitalization: For close observation and supportive care, the majority of people with acute pancreatitis need to be hospitalized.
In order to give the pancreas time to rest, patients are frequently required to fast and receive intravenous (IV) fluids. Through an IV, they get water and nutrition.
Pain management: A key component of treatment is the reduction of pain. To reduce pain, medications, such as analgesics, are given.
Taking Care of the Root Cause
Gallstones: If gallstones are the underlying issue, treatment options include cholecystectomy, the removal of the gallbladder.
Alcohol: Patients are recommended to refrain from drinking if alcohol is the trigger.
Infections: If there is evidence of an infection, antibiotics may be recommended.
Nutritional Support: A gradual switch to a soft diet may be started when the patient’s condition gets better.
Endoscopic or surgical interventions may be required to drain or remove the afflicted areas in cases of problems including pseudocysts, diseased tissue, or blocked ducts.
Diabetes care: Patients will need continuing diabetes care, which may involve insulin therapy, if diabetes arises as a result of pancreas impairment.
Adapting a balanced diet and avoiding alcohol (if it was a significant factor) are only a few lifestyle changes that those who have experienced acute pancreatitis should make.
VIII. Recovery and Prognosis
The severity of acute pancreatitis and if complications arise affect the prognosis. With the right care, mild instances of acute pancreatitis frequently get better in a few days to a week, and the outlook is usually good.
Especially when accompanied by infection, pancreatic necrosis, or organ failure, severe cases can be fatal. For better results, early diagnosis and management are essential.
A gradual return to daily routine and an emphasis on maintaining a healthy lifestyle are sometimes required for acute pancreatitis recovery.
IX. Taking Steps to Avoid Acute Pancreatitis
Addressing risk factors and changing one’s lifestyle are necessary for preventing acute pancreatitis. Here are some precautions to take:
Moderate Alcohol Use: If alcohol use was a contributing issue, cut back on your consumption or stop drinking completely.
Manage gallstones: If you have gallstones, talk to your doctor about your treatment choices.
Reduce High Blood Lipid Levels: If you have hypertriglyceridemia or hypercalcemia, manage these disorders in conjunction with your healthcare professional.
Maintain a Healthy Diet: A diet high in fruits, vegetables, and whole grains, low in saturated fats, can help lower the incidence of gallstones.
Drink plenty of water to stay hydrated and to avoid the development of gallstones.
Avoid Smoking: Since smoking increases the risk of pancreatic illness, quitting is a good idea.
Conclusion:-
Acute pancreatitis is a severe illness that needs to be treated right away. It is essential for both those at risk and healthcare professionals to comprehend the conditions causes, symptoms, diagnosis, and available treatments. Many cases of acute pancreatitis can be efficiently controlled, and the risk of complications is reduced, with prompt treatment and early intervention. Prevention of this unpleasant and potentially fatal condition can be greatly aided by maintaining a healthy lifestyle and addressing risk factors.